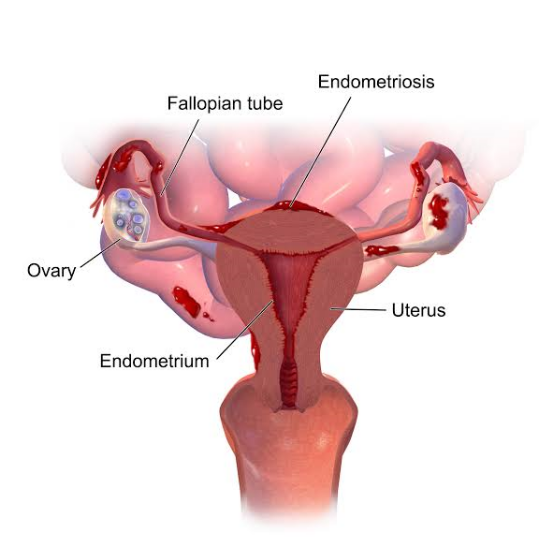
Endometriosis is a chronic and often painful gynecological condition that affects millions of women worldwide. It occurs when tissue similar to the uterine lining (endometrium) grows outside the uterus, typically in the pelvic area, causing inflammation and discomfort. This informative article aims to shed light on endometriosis, discussing its causes, common symptoms, diagnostic approaches, and available management options. By increasing awareness and understanding of this condition, women can seek timely medical attention and access appropriate care to improve their quality of life.
Causes and Risk Factors:
The exact cause of endometriosis remains unclear, but several factors contribute to its development, including:
- Retrograde Menstruation: Menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity, where these cells implant
and grow. - Genetic Predisposition: A family history of endometriosis increases the likelihood of developing the condition.
- Hormonal Imbalances: Abnormal hormone levels, particularly estrogen, may promote the growth of endometrial tissue outside the uterus.
- Immune System Dysfunction: A compromised immune response may fail to
recognize and eliminate endometrial tissue growing in the wrong locations.
Common Symptoms:
Endometriosis symptoms can vary widely among women, and some may experience mild discomfort, while others may endure severe pain. Common signs and symptoms include:
- Pelvic Pain: Chronic pelvic pain, often during menstruation, is a hallmark symptom of endometriosis. The pain may radiate to the lower back and legs.
- Dysmenorrhea: Painful periods, characterized by severe menstrual cramps, are a common complaint among women with endometriosis.
- Painful Intercourse: Pain during sexual intercourse, known as dyspareunia, can be a distressing symptom for women with endometriosis.
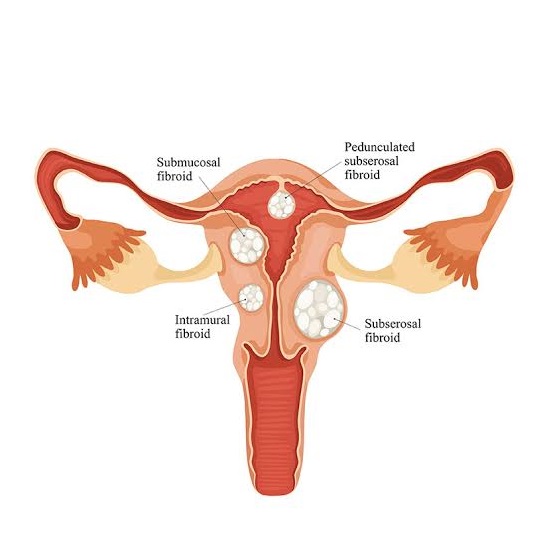
- Heavy Menstrual Bleeding: Some women with endometriosis may experience excessive menstrual bleeding.
- Infertility: Endometriosis can cause fertility challenges due to adhesions and inflammation affecting the reproductive organs.
Diagnosis:
Diagnosing endometriosis can be challenging, as symptoms may overlap with other conditions. A comprehensive evaluation typically includes:
- Medical History and Physical Examination: A detailed medical history, including menstrual patterns and pain characteristics, is essential. A pelvic exam can help identify any abnormal masses or tenderness.
- Imaging Studies: Ultrasound or MRI can provide visual clues about endometrial growths.
- Laparoscopy: The gold standard for diagnosing endometriosis involves a minimally invasive procedure called laparoscopy. A thin tube with a camera (laparoscope) is inserted into the abdomen to visualize and biopsy any abnormal tissue.
Management Options:
The management of endometriosis aims to alleviate symptoms, improve fertility (if desired), and enhance overall well-being. Treatment options include:
- Pain Medications: Over-the-counter pain relievers or prescription medications may help manage pelvic pain and menstrual discomfort
- Hormonal Therapy: Hormonal medications like birth control pills, progestins, or gonadotropin-releasing hormone agonists can suppress hormone fluctuations and reduce endometrial growth.
- Surgery: Laparoscopic surgery can be performed to remove endometrial tissue, adhesions, and cysts, improving symptoms and fertility.
- Assisted Reproductive Techniques: In cases of infertility, assisted reproductive technologies like in vitro fertilization (IVF) may help achieve pregnancy.